
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
- Pioglitazone as Add-on THERAPY in Patients with Type 2 Diabetes Mellitus Inadequately Controlled with Dapagliflozin and Metformin: Double-Blind, Randomized, Placebo-Controlled Trial
- Ji Hye Heo, Kyung Ah Han, Jun Hwa Hong, Hyun-Ae Seo, Eun-Gyoung Hong, Jae Myung Yu, Hye Seung Jung, Bong-Soo Cha
- Received September 1, 2023 Accepted October 25, 2023 Published online February 2, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0314 [Epub ahead of print]
- 1,203 View
- 114 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
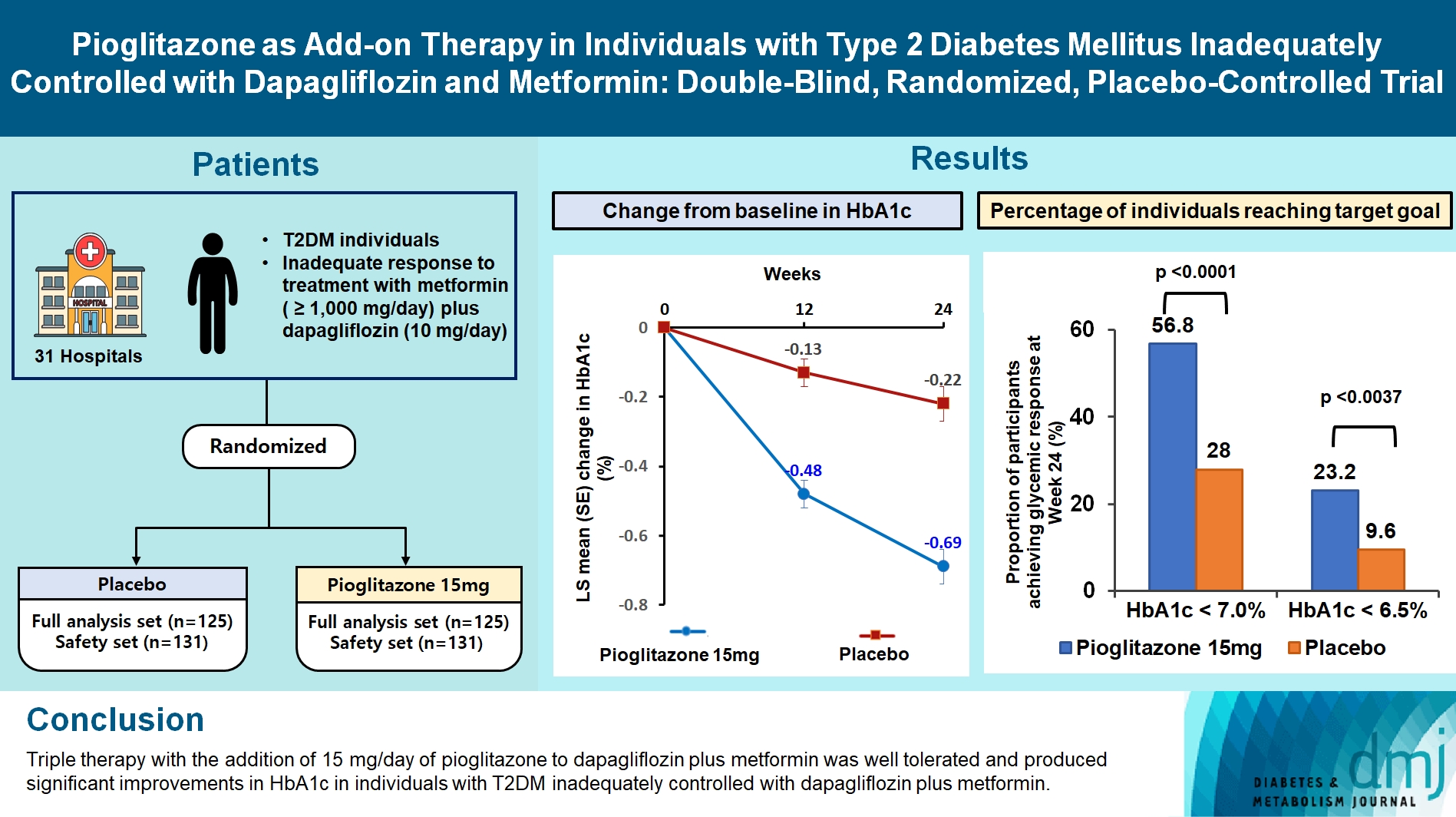
This study assessed the efficacy and safety of triple therapy with pioglitazone 15 mg add-on versus placebo in patients with type 2 diabetes mellitus (T2DM) inadequately controlled with metformin and dapagliflozin.
Methods
In this multicenter, double-blind, randomized, phase 3 study, patients with T2DM with an inadequate response to treatment with metformin (≥1,000 mg/day) plus dapagliflozin (10 mg/day) were randomized to receive additional pioglitazone 15 mg/day (n=125) or placebo (n=125) for 24 weeks. The primary endpoint was the change in glycosylated hemoglobin (HbA1c) levels from baseline to week 24 (ClinicalTrials.gov identifier: NCT05101135).
Results
At week 24, the adjusted mean change from baseline in HbA1c level compared with placebo was significantly greater with pioglitazone treatment (–0.47%; 95% confidence interval, –0.61 to –0.33; P<0.0001). A greater proportion of patients achieved HbA1c <7% or <6.5% at week 24 with pioglitazone compared to placebo as add-on to 10 mg dapagliflozin and metformin (56.8% vs. 28% for HbA1c <7%, and 23.2% vs. 9.6% for HbA1c <6.5%; P<0.0001 for all). The addition of pioglitazone also significantly improved triglyceride, highdensity lipoprotein cholesterol levels, and homeostatic model assessment of insulin resistance levels, while placebo did not. The incidence of treatment-emergent adverse events was similar between the groups, and the incidence of fluid retention-related side effects by pioglitazone was low (1.5%).
Conclusion
Triple therapy with the addition of 15 mg/day of pioglitazone to dapagliflozin plus metformin was well tolerated and produced significant improvements in HbA1c in patients with T2DM inadequately controlled with dapagliflozin plus metformin.
- Complications
- Deterioration of Sleep Quality According to Glycemic Status
- Myung Haeng Hur, Mi-Kyoung Lee, Kayeon Seong, Jun Hwa Hong
- Diabetes Metab J. 2020;44(5):679-686. Published online April 17, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0125
- 4,875 View
- 113 Download
- 5 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
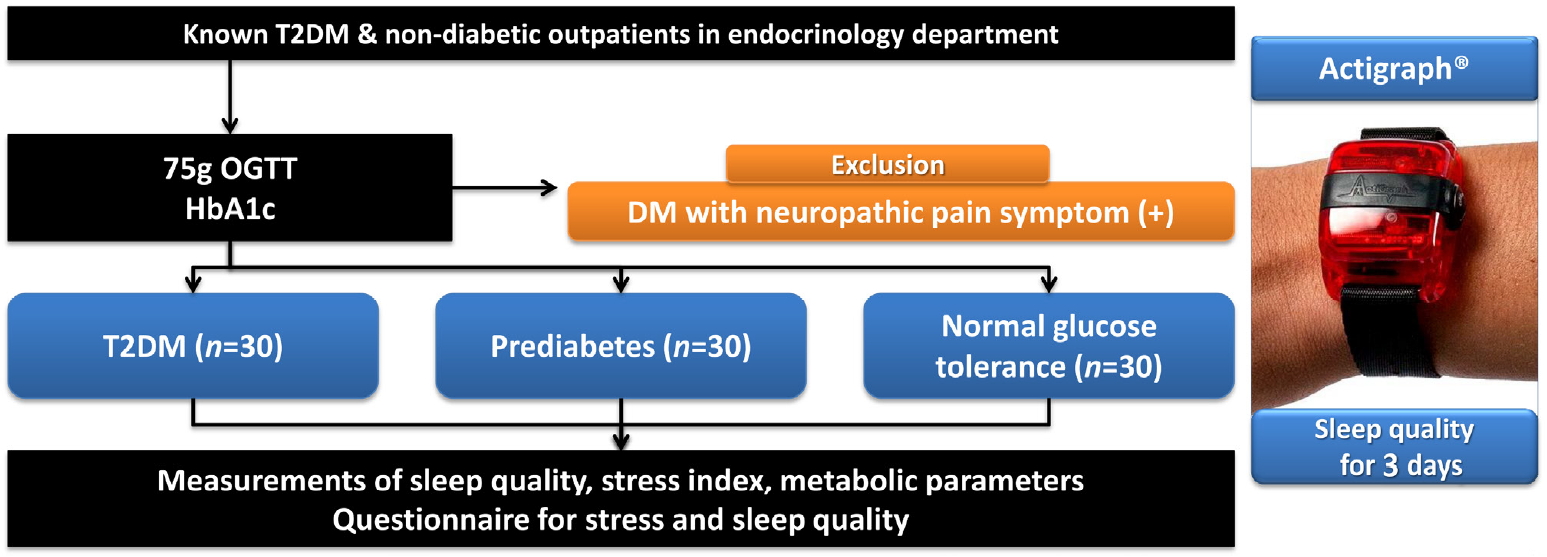
ePub Background Type 2 diabetes mellitus (T2DM) is a progressive disease with multiple complications. The present study aimed to determine the effects of glycemic status on sleep quality in individuals with T2DM, prediabetes, and normal glucose tolerance (NGT).
Methods A total of 90 participants were categorized into three groups, T2DM (
n =30), prediabetes (n =30), and NGT (n =30). Objective sleep quality was measured with the actigraph wrist-worn device over 3 nights and subjective sleep quality was evaluated with a questionnaire.Results The duration of diabetes in the T2DM group was 2.23 years and the glycosylated hemoglobin (HbA1c) levels in the T2DM, prediabetes, and NGT groups were 7.83%, 5.80%, and 5.31%, respectively. Sleep efficiency decreased across the T2DM, prediabetes, and NGT groups (86.25%, 87.99%, and 90.22%, respectively;
P =0.047). Additionally, HbA1c levels revealed a significant negative correlation with sleep efficiency (r =−0.348,P =0.001). The sleep quality questionnaire results were similar among the three groups.Conclusion Although the participants in the present study were not necessarily conscious of their sleep disturbances, deterioration in sleep quality progressed according to glycemic status.
-
Citations
Citations to this article as recorded by- Risk factors of non communicable diseases among recently diagnosed diabetic patients in a tertiary care Hospital
Yusra Amin, Sonia Mushtaq, Rukhsana Farooq
Indian Journal of Clinical Anatomy and Physiology.2024; 10(4): 205. CrossRef - Metabolic health tracking using Ultrahuman M1 continuous glucose monitoring platform in non- and pre-diabetic Indians: a multi-armed observational study
Monik Chaudhry, Mohit Kumar, Vatsal Singhal, Bhuvan Srinivasan
Scientific Reports.2024;[Epub] CrossRef - Relation between sleep quality and glycemic control among type 2 diabetic patients
Asmaa Ali Elsayed Ali
Frontiers of Nursing.2023; 10(1): 115. CrossRef - Heart rate variability in different sleep stages is associated with metabolic function and glycemic control in type 2 diabetes mellitus
Wenquan Cheng, Hongsen Chen, Leirong Tian, Zhimin Ma, Xingran Cui
Frontiers in Physiology.2023;[Epub] CrossRef - Association Between Diabetic Retinopathy and Insomnia Risk: A Nationwide Population-Based Study
Yoo Hyun Um, Tae-Won Kim, Jong-Hyun Jeong, Seung-Chul Hong, Ho-Jun Seo, Kyung-Do Han
Frontiers in Endocrinology.2022;[Epub] CrossRef - Nutritional Biomarkers and Factors Correlated with Poor Sleep Status among Young Females: A Case-Control Study
Sara AL-Musharaf, Lama AlAjllan, Ghadeer Aljuraiban, Munirah AlSuhaibani, Noura Alafif, Syed Danish Hussain
Nutrients.2022; 14(14): 2898. CrossRef - The impact of sleep disorders on microvascular complications in patients with type 2 diabetes (SLEEP T2D): the protocol of a cohort study and feasibility randomised control trial
Christina Antza, Ryan Ottridge, Smitaa Patel, Gemma Slinn, Sarah Tearne, Matthew Nicholls, Brendan Cooper, Asad Ali, Abd A. Tahrani
Pilot and Feasibility Studies.2021;[Epub] CrossRef - Early Development of Bidirectional Associations between Sleep Disturbance and Diabetes
Yongin Cho
Diabetes & Metabolism Journal.2020; 44(5): 668. CrossRef
- Risk factors of non communicable diseases among recently diagnosed diabetic patients in a tertiary care Hospital
- Letter: The Necessity of the Simple Tests for Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus Patients without Neuropathic Symptoms in Clinical Practice (
Diabetes Metab J 2018;42:442-6) - Jun Hwa Hong
- Diabetes Metab J. 2018;42(6):544-545. Published online December 17, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0238
- 2,714 View
- 35 Download
- Clinical Care/Education
- Patient Understanding of Hypoglycemia in Tertiary Referral Centers
- Nan Hee Cho, Nam Kyung Kim, Eugene Han, Jun Hwa Hong, Eon Ju Jeon, Jun Sung Moon, Mi Hae Seo, Ji Eun Lee, Hyun-Ae Seo, Mi-Kyung Kim, Hye Soon Kim
- Diabetes Metab J. 2018;42(1):43-52. Published online February 23, 2018
- DOI: https://doi.org/10.4093/dmj.2018.42.1.43
- 4,583 View
- 54 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Hypoglycemia is an important complication in the treatment of patients with diabetes. We surveyed the insight by patients with diabetes into hypoglycemia, their hypoglycemia avoidance behavior, and their level of worry regarding hypoglycemia.
Methods A survey of patients with diabetes, who had visited seven tertiary referral centers in Daegu or Gyeongsangbuk-do, Korea, between June 2014 and June 2015, was conducted. The survey contained questions about personal history, symptoms, educational experience, self-management, and attitudes about hypoglycemia.
Results Of 758 participants, 471 (62.1%) had experienced hypoglycemia, and 250 (32.9%) had experienced hypoglycemia at least once in the month immediately preceding the study. Two hundred and forty-two (31.8%) of the participants had received hypoglycemia education at least once, but only 148 (19.4%) knew the exact definition of hypoglycemia. Hypoglycemic symptoms identified by the participants were dizziness (55.0%), sweating (53.8%), and tremor (40.8%). They mostly chose candy (62.1%), chocolate (37.7%), or juice (36.8%) as food for recovering hypoglycemia. Participants who had experienced hypoglycemia had longer duration of diabetes and a higher proportion of insulin usage. The mean scores for hypoglycemia avoidance behavior and worry about hypoglycemia were 21.2±10.71 and 23.38±13.19, respectively. These scores tended to be higher for participants with higher than 8% of glycosylated hemoglobin, insulin use, and experience of emergency room visits.
Conclusion Many patients had experienced hypoglycemia and worried about it. We recommend identifying patients that are anxious about hypoglycemia and educating them about what to do when they develop hypoglycemic symptoms, especially those who have a high risk of hypoglycemia.
-
Citations
Citations to this article as recorded by- Severe Hypoglycemia Increases Dementia Risk and Related Mortality: A Nationwide, Population-based Cohort Study
Eugene Han, Kyung-do Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Seung-Hyun Ko, Yong-ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(5): e1976. CrossRef - Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus
Soo-Yeon Choi, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 263. CrossRef - Severe hypoglycemia and the risk of end stage renal disease in type 2 diabetes
Jae-Seung Yun, Yong-Moon Park, Kyungdo Han, Hyung-Wook Kim, Seon-Ah Cha, Yu-Bae Ahn, Seung-Hyun Ko
Scientific Reports.2021;[Epub] CrossRef - Response: Patient Understanding of Hypoglycemia in Tertiary Referral Centers (Diabetes Metab J 2018;42:43-52)
Nan Hee Cho, Hye Soon Kim
Diabetes & Metabolism Journal.2018; 42(2): 175. CrossRef - Letter: Patient Understanding of Hypoglycemia in Tertiary Referral Centers (Diabetes Metab J 2018;42:43-52)
Jae-Han Jeon
Diabetes & Metabolism Journal.2018; 42(2): 173. CrossRef
- Severe Hypoglycemia Increases Dementia Risk and Related Mortality: A Nationwide, Population-based Cohort Study
- Response: GDF15 Is a Novel Biomarker for Impaired Fasting Glucose (
Diabetes Metab J 2014;38:472-9) - Jun Hwa Hong, Bon Jeong Ku, Minho Shong
- Diabetes Metab J. 2015;39(1):84-86. Published online February 16, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.1.84
- 2,908 View
- 27 Download
- GDF15 Is a Novel Biomarker for Impaired Fasting Glucose
- Jun Hwa Hong, Hyo Kyun Chung, Hye Yoon Park, Kyong-Hye Joung, Ju Hee Lee, Jin Gyu Jung, Koon Soon Kim, Hyun Jin Kim, Bon Jeong Ku, Minho Shong
- Diabetes Metab J. 2014;38(6):472-479. Published online December 15, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.6.472
- 5,481 View
- 75 Download
- 67 Web of Science
- 63 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Growth differentiation factor-15 (GDF15) is a protein that belongs to the transforming growth factor β superfamily. An elevated serum level of GDF15 was found to be associated with type 2 diabetes mellitus (T2DM). T2DM is an inflammatory disease that progresses from normal glucose tolerance (NGT) to impaired fasting glucose (IFG). Hence, we aimed to validate the relationship between GDF15 and IFG.
Methods The participants were divided into the following three groups: NGT (
n =137), IFG (n =29), and T2DM (n =75). The controls and T2DM outpatients visited the hospital for routine health check-ups. We used fasting blood glucose to detect IFG in nondiabetic patients. We checked the body mass index (BMI), C-reactive protein level, metabolic parameters, and fasting serum GDF15 level.Results Age, BMI, triglyceride, insulin, glucose, homeostatic model assessment-insulin resistance (HOMA-IR), and GDF15 levels were elevated in the IFG and T2DM groups compared to the NGT group. In the correlation analysis between metabolic parameters and GDF15, age and HOMA-IR had a significant positive correlation with GDF15 levels. GDF15 significantly discriminated between IFG and NGT, independent of age, BMI, and HOMA-IR. The serum levels of GDF15 were more elevated in men than in women. As a biomarker for IFG based on the receiver operating characteristic curve analysis, the cutoff value of GDF15 was 510 pg/mL in males and 400 pg/mL in females.
Conclusion GDF15 had a positive correlation with IR independent of age and BMI, and the serum level of GDF15 was increased in the IFG and T2DM groups. GDF15 may be a novel biomarker for detecting IFG in nondiabetic patients.
-
Citations
Citations to this article as recorded by- Effect of a 6-Week Carbohydrate-Reduced High-Protein Diet on Levels of FGF21 and GDF15 in People With Type 2 Diabetes
Michael M Richter, Mads N Thomsen, Mads J Skytte, Sasha A S Kjeldsen, Amirsalar Samkani, Jan Frystyk, Faidon Magkos, Jens J Holst, Sten Madsbad, Thure Krarup, Steen B Haugaard, Nicolai J Wewer Albrechtsen
Journal of the Endocrine Society.2024;[Epub] CrossRef - Serum Growth Differentiation Factor 15 Levels Predict the Incidence of Frailty among Patients with Cardiometabolic Diseases
Kazuhito Oba, Joji Ishikawa, Yoshiaki Tamura, Yasunori Fujita, Masafumi Ito, Ai Iizuka, Yoshinori Fujiwara, Remi Kodera, Kenji Toyoshima, Yuko Chiba, Masashi Tanaka, Atsushi Araki
Gerontology.2024; : 1. CrossRef - Growth differentiation factor 15 and malnutrition in older adults
Nazanin Rostami, Blanca Fabre-Estremera, Antonio Buño-Soto, José R Banegas, Fernando Rodríguez-Artalejo, Rosario Ortolá
The Journal of nutrition, health and aging.2024; 28(6): 100230. CrossRef - Evaluation of the relation between subclinical systolic dysfunction defined by four-dimensional speckle-tracking echocardiography and growth differentiation factor-15 levels in patients with acromegaly
Busra Firlatan, Ugur Nadir Karakulak, Vedat Hekimsoy, Burcin Gonul Iremli, Incilay Lay, Deniz Yuce, Selcuk Dagdelen, Giray Kabakci, Tomris Erbas
Hormones.2024;[Epub] CrossRef - Exploration of meteorin-like peptide (metrnl) predictors in type 2 diabetic patients: the potential role of irisin, and other biochemical parameters
Yaser Khajebishak, Amir Hossein Faghfouri, Ali Soleimani, Sadra Madani, Laleh Payahoo
Hormone Molecular Biology and Clinical Investigation.2023; 44(2): 127. CrossRef - Relationship between meteorin-like peptide (Metrnl) serum levels and inflammatory cytokines, oxidative stress biomarkers and body composition parameters in type 2 diabetes patients
Yaser Khajebishak, Sadra Madani, Amir Hossein Faghfouri, Ali Soleimani, Sara Ilaei, Said Peyrovi, Laleh Payahoo
Nutrition & Food Science.2023; 53(5): 861. CrossRef - Effects of acute exercise and exercise training on plasma GDF15 concentrations and associations with appetite and cardiometabolic health in individuals with overweight or obesity – A secondary analysis of a randomized controlled trial
Jonas Salling Quist, Anders Bue Klein, Kristine Færch, Kristine Beaulieu, Mads Rosenkilde, Anne Sofie Gram, Anders Sjödin, Signe Torekov, Bente Stallknecht, Christoffer Clemmensen, Martin Bæk Blond
Appetite.2023; 182: 106423. CrossRef - Significant increase of serum extracellular vesicle-packaged growth differentiation factor 15 in type 2 diabetes mellitus: a cross-sectional study
Wen Zhao, Xinwei Li, Xinxin Li, Lu Peng, Yu Li, Yunhui Du, Jianxun He, Yanwen Qin, Huina Zhang
European Journal of Medical Research.2023;[Epub] CrossRef - Association between growth differentiation factor 15 levels and gestational diabetes mellitus: A combined analysis
Yi-Cheng Lu, Song-Liang Liu, Yu-Shan Zhang, Fei Liang, Xiao-Yan Zhu, Yue Xiao, Jing Wang, Cong Ding, Sudipta Banerjee, Jie-Yun Yin, Qiu-Ping Ma
Frontiers in Endocrinology.2023;[Epub] CrossRef - Metformin triggers a kidney GDF15-dependent area postrema axis to regulate food intake and body weight
Song-Yang Zhang, Kyla Bruce, Zahra Danaei, Rosa J.W. Li, Daniel R. Barros, Rachel Kuah, Yu-Mi Lim, Laura H. Mariani, David Z. Cherney, Jennifer F.M. Chiu, Heather N. Reich, Tony K.T. Lam
Cell Metabolism.2023; 35(5): 875. CrossRef - Growth differentiation factor 15 (GDF-15) in endocrinology
Pedro Iglesias, Ramona A. Silvestre, Juan J. Díez
Endocrine.2023; 81(3): 419. CrossRef - Identification of biomarkers for glycaemic deterioration in type 2 diabetes
Roderick C. Slieker, Louise A. Donnelly, Elina Akalestou, Livia Lopez-Noriega, Rana Melhem, Ayşim Güneş, Frederic Abou Azar, Alexander Efanov, Eleni Georgiadou, Hermine Muniangi-Muhitu, Mahsa Sheikh, Giuseppe N. Giordano, Mikael Åkerlund, Emma Ahlqvist, A
Nature Communications.2023;[Epub] CrossRef - Metabolic syndrome and Growth Differentiation Factor 15 in older adults
Adrián Carballo-Casla, Esther García-Esquinas, Antonio Buño-Soto, Ellen A. Struijk, Esther López-García, Fernando Rodríguez-Artalejo, Rosario Ortolá
GeroScience.2022; 44(2): 867. CrossRef - Associations between GDF15 Levels and Pre-Diabetes in Non-Obese Subjects
Hao-Chang Hung, Hung-Tsung Wu, Ching-Han Lin, Hsuan-Wen Chou, Horng-Yih Ou, Chih-Jen Chang
Journal of Investigative Medicine.2022; 70(1): 79. CrossRef - Growth Differentiation Factor-15 as a Biomarker of Obese Pre-diabetes and Type 2 Diabetes Mellitus in Indian Subjects: A Case-control Study
Dipayan Roy, Purvi Purohit, Anupama Modi, Manoj Khokhar, Ravindra Kumar Gayaprasad Shukla, Ramkaran Chaudhary, Shrimanjunath Sankanagoudar, Praveen Sharma
Current Diabetes Reviews.2022;[Epub] CrossRef - Growth Differentiation Factor 15 Protects SH-SY5Y Cells From Rotenone-Induced Toxicity by Suppressing Mitochondrial Apoptosis
Peizheng Li, Hongbo Lv, Bohan Zhang, Ruonan Duan, Xiufang Zhang, Pengfei Lin, Chengyuan Song, Yiming Liu
Frontiers in Aging Neuroscience.2022;[Epub] CrossRef - GDF-15 as a Therapeutic Target of Diabetic Complications Increases the Risk of Gallstone Disease: Mendelian Randomization and Polygenic Risk Score Analysis
Lili Yu, Yajing Zhou, Lijuan Wang, Xuan Zhou, Jing Sun, Jiarui Xiao, Xiaolin Xu, Susanna C. Larsson, Shuai Yuan, Xue Li
Frontiers in Genetics.2022;[Epub] CrossRef - Sex-specific modulation of circulating growth differentiation factor-15 in patients with type 2 diabetes and/or obesity
Mohamed Asrih, Flore Sinturel, Richard Dubos, Idris Guessous, Zoltan Pataky, Charna Dibner, François R Jornayvaz, Karim Gariani
Endocrine Connections.2022;[Epub] CrossRef - Raised circulating soluble growth differentiation factor 15 is negatively associated with testosterone level in hypogonadic men with type 2 diabetes
Yufeng Mei, Yongnan Lyu, Juan Le, Di Li, Hang Liu, Zhiming Zhao, Yan Li
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - NCAM1 and GDF15 are biomarkers of Charcot-Marie-Tooth disease in patients and mice
Matthew J Jennings, Alexia Kagiava, Leen Vendredy, Emily L Spaulding, Marina Stavrou, Denisa Hathazi, Anika Grüneboom, Vicky De Winter, Burkhard Gess, Ulrike Schara, Oksana Pogoryelova, Hanns Lochmüller, Christoph H Borchers, Andreas Roos, Robert W Burges
Brain.2022; 145(11): 3999. CrossRef - Metformin and growth differentiation factor 15 (GDF15) in type 2 diabetes mellitus: A hidden treasure
Hayder M. Al‐kuraishy, Ali I. Al‐Gareeb, Athanasios Alexiou, Marios Papadakis, Eman Hassan Nadwa, Sarah M. Albogami, Mohammed Alorabi, Hebatallah M. Saad, Gaber El‐Saber Batiha
Journal of Diabetes.2022; 14(12): 806. CrossRef - GDF15 is an exercise-induced hepatokine regulated by glucagon and insulin in humans
Peter Plomgaard, Jakob S. Hansen, Logan K. Townsend, Anders Gudiksen, Niels H. Secher, Jens O. Clemmesen, Rene K. Støving, Jens P. Goetze, David C. Wright, Henriette Pilegaard
Frontiers in Endocrinology.2022;[Epub] CrossRef - A study of serum growth differentiation factor 15 in Indian women with and without gestational diabetes mellitus in the third trimester of pregnancy and its association with pro-inflammatory markers and glucose metabolism
Sudipta Banerjee, Rana Bhattacharjee, Amitabh Sur, Pieu Adhikary, Subhankar Chowdhury
Diabetology International.2021; 12(3): 254. CrossRef - Growth Differentiation Factor 15 is a Cancer Cell-Induced Mitokine That Primes Thyroid Cancer Cells for Invasiveness
Yea Eun Kang, Jin Man Kim, Mi Ae Lim, Seong Eun Lee, Shinae Yi, Jung Tae Kim, Chan Oh, Lihua Liu, Yanli Jin, Seung-Nam Jung, Ho-Ryun Won, Jae Won Chang, Jeong Ho Lee, Hyun Jung Kim, Hyun Yong Koh, Sangmi Jun, Sun Wook Cho, Minho Shong, Bon Seok Koo
Thyroid.2021; 31(5): 772. CrossRef - The GDF15-GFRAL Pathway in Health and Metabolic Disease: Friend or Foe?
Samuel N. Breit, David A. Brown, Vicky Wang-Wei Tsai
Annual Review of Physiology.2021; 83(1): 127. CrossRef - Associations of GDF-15 and GDF-15/adiponectin ratio with odds of type 2 diabetes in the Chinese population
Xiaoying Wu, Wenting Xuan, Lili You, Hong Lian, Feng Li, Xiaoyun Zhang, Qingyu Chen, Kan Sun, Chaogang Chen, Mingtong Xu, Yan Li, Li Yan, Xiuwei Zhang, Meng Ren
Endocrine.2021; 72(2): 423. CrossRef - Decreased serum growth differentiation factor 15 levels after lifestyle intervention in patients with newly diagnosed type 2 diabetes mellitus
Xingxing He, Jiaorong Su, Xiaojing Ma, Jingyi Lu, Yufei Wang, Jun Yin, Yuqian Bao, Gang Hu, Jian Zhou
Obesity Medicine.2021; 24: 100345. CrossRef - The anti-diabetic effects of NAG-1/GDF15 on HFD/STZ-induced mice
Pattawika Lertpatipanpong, Jaehak Lee, Ilju Kim, Thomas Eling, Seung Yeon Oh, Je Kyung Seong, Seung Joon Baek
Scientific Reports.2021;[Epub] CrossRef - The Regulation of Circulating Hepatokines by Fructose Ingestion in Humans
Michael M Richter, Peter Plomgaard
Journal of the Endocrine Society.2021;[Epub] CrossRef - GDF15: emerging biology and therapeutic applications for obesity and cardiometabolic disease
Dongdong Wang, Emily A. Day, Logan K. Townsend, Djordje Djordjevic, Sebastian Beck Jørgensen, Gregory R. Steinberg
Nature Reviews Endocrinology.2021; 17(10): 592. CrossRef - High Fat, High Sugar Diet and DJOS Bariatric Surgery Influence Plasma Levels of Fetuin-B, Growth Differentiation Factor-15, and Pentraxin 3 in Diet-Induced Obese Sprague–Dawley Rats
Jakub Poloczek, Monika Tarnawska, Elżbieta Chełmecka, Piotr Łaszczyca, Janusz Gumprecht, Dominika Stygar
Nutrients.2021; 13(10): 3632. CrossRef - Serum growth differentiation factor 15 level is associated with muscle strength and lower extremity function in older patients with cardiometabolic disease
Kazuhito Oba, Joji Ishikawa, Yoshiaki Tamura, Yasunori Fujita, Masafumi Ito, Ai Iizuka, Yoshinori Fujiwara, Remi Kodera, Ayumi Toba, Kenji Toyoshima, Yuko Chiba, Seijiro Mori, Masashi Tanaka, Hideki Ito, Kazumasa Harada, Atsushi Araki
Geriatrics & Gerontology International.2020; 20(10): 980. CrossRef - Growth differentiation factor 15 (GDF-15) is a potential biomarker of both diabetic kidney disease and future cardiovascular events in cohorts of individuals with type 2 diabetes: a proteomics approach
Axel C. Carlsson, Christoph Nowak, Lars Lind, Carl Johan Östgren, Fredrik H. Nyström, Johan Sundström, Juan Jesus Carrero, Ulf Riserus, Erik Ingelsson, Tove Fall, Johan Ärnlöv
Upsala Journal of Medical Sciences.2020; 125(1): 37. CrossRef - Elevated Plasma Growth and Differentiation Factor 15 Is Associated With Slower Gait Speed and Lower Physical Performance in Healthy Community-Dwelling Adults
Richard D Semba, Marta Gonzalez-Freire, Toshiko Tanaka, Angelique Biancotto, Pingbo Zhang, Michelle Shardell, Ruin Moaddel, Luigi Ferrucci, Anne Newman
The Journals of Gerontology: Series A.2020; 75(1): 175. CrossRef - Circulating Cardiac Biomarkers in Diabetes Mellitus: A New Dawn for Risk Stratification—A Narrative Review
Alexander E. Berezin, Alexander A. Berezin
Diabetes Therapy.2020; 11(6): 1271. CrossRef - Deterioration of Sleep Quality According to Glycemic Status
Myung Haeng Hur, Mi-Kyoung Lee, Kayeon Seong, Jun Hwa Hong
Diabetes & Metabolism Journal.2020; 44(5): 679. CrossRef - Effects of plant and animal high protein diets on immune-inflammatory biomarkers: A 6-week intervention trial
Mariya Markova, Liselot Koelman, Silke Hornemann, Olga Pivovarova, Stephanie Sucher, Juergen Machann, Natalia Rudovich, Ralph Thomann, Rosemarie Schneeweiss, Sascha Rohn, Andreas F.H. Pfeiffer, Krasimira Aleksandrova
Clinical Nutrition.2020; 39(3): 862. CrossRef - Effect of sleeve gastrectomy on plasma growth differentiation factor-15 (GDF15) in human
Ponnie Robertlee Dolo, Libin Yao, Peng Peng Liu, Jason Widjaja, Song Meng, Chao Li, Xiaocheng Zhu
The American Journal of Surgery.2020; 220(3): 725. CrossRef - Prognostication of clinical outcomes in diabetes mellitus: Emerging role of cardiac biomarkers
Alexander E. Berezin
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(2): 995. CrossRef - Effect of bariatric surgery on plasma GDF15 in humans
Maximilian Kleinert, Kirstine N. Bojsen-Møller, Nils B. Jørgensen, Maria S. Svane, Christoffer Martinussen, Bente Kiens, Jørgen F.P. Wojtaszewski, Sten Madsbad, Erik A. Richter, Christoffer Clemmensen
American Journal of Physiology-Endocrinology and Metabolism.2019; 316(4): E615. CrossRef - Regulation of Systemic Glucose Homeostasis by T Helper Type 2 Cytokines
Yea Eun Kang, Hyun Jin Kim, Minho Shong
Diabetes & Metabolism Journal.2019; 43(5): 549. CrossRef - GDF15 reflects beta cell function in obese patients independently of the grade of impairment of glucose metabolism
M.H. Schernthaner-Reiter, B.K. Itariu, M. Krebs, M. Promintzer-Schifferl, T.M. Stulnig, A. Tura, C.H. Anderwald, M. Clodi, B. Ludvik, G. Pacini, A. Luger, G. Vila
Nutrition, Metabolism and Cardiovascular Diseases.2019; 29(4): 334. CrossRef - Growth differentiation factor 15: A novel biomarker with high clinical potential
Stéphanie Desmedt, Valérie Desmedt, Leen De Vos, Joris R. Delanghe, Reinhart Speeckaert, Marijn M. Speeckaert
Critical Reviews in Clinical Laboratory Sciences.2019; 56(5): 333. CrossRef - Hepatokines—a novel group of exercise factors
Cora Weigert, Miriam Hoene, Peter Plomgaard
Pflügers Archiv - European Journal of Physiology.2019; 471(3): 383. CrossRef - Association between MIC-1 and Type 2 Diabetes: A Combined Analysis
Jianan Lu, Yue Zhang, Xingxuan Dong, Jiawen Lu, Chen Zhang, Jieyu Liu, Qingzhou Yu, Haoyue Teng, Qingkui Yao, Jieyun Yin, Liqiang Qin
Disease Markers.2019; 2019: 1. CrossRef - The mitochondrial unfolded protein response and mitohormesis: a perspective on metabolic diseases
Hyon-Seung Yi, Joon Young Chang, Minho Shong
Journal of Molecular Endocrinology.2018; 61(3): R91. CrossRef - Towards frailty biomarkers: Candidates from genes and pathways regulated in aging and age-related diseases
Ana Luisa Cardoso, Adelaide Fernandes, Juan Antonio Aguilar-Pimentel, Martin Hrabě de Angelis, Joana Ribeiro Guedes, Maria Alexandra Brito, Saida Ortolano, Giovambattista Pani, Sophia Athanasopoulou, Efstathios S. Gonos, Markus Schosserer, Johannes Grilla
Ageing Research Reviews.2018; 47: 214. CrossRef - Serum Meteorin-like protein levels decreased in patients newly diagnosed with type 2 diabetes
Ju Hee Lee, Yea Eun Kang, Ji Min Kim, Sorim Choung, Kyong Hye Joung, Hyun Jin Kim, Bon Jeong Ku
Diabetes Research and Clinical Practice.2018; 135: 7. CrossRef - Growth differentiation factor 15 predicts advanced fibrosis in biopsy‐proven non‐alcoholic fatty liver disease
Bo Kyung Koo, Sung Hee Um, Dong Soo Seo, Sae Kyung Joo, Jeong Mo Bae, Jeong Hwan Park, Mee Soo Chang, Jung Ho Kim, Jieun Lee, Won‐Il Jeong, Won Kim
Liver International.2018; 38(4): 695. CrossRef - Serum Growth Differentiation Factor 15 in Parkinson Disease
Xiaomei Yao, Dong Wang, Lei Zhang, Lingling Wang, Zhenxiang Zhao, Si Chen, Xiaotang Wang, Tao Yue, Yiming Liu
Neurodegenerative Diseases.2017; 17(6): 251. CrossRef - GDF15 deficiency exacerbates chronic alcohol- and carbon tetrachloride-induced liver injury
Hyo Kyun Chung, Jung Tae Kim, Hyeon-Woo Kim, Minjoo Kwon, So Yeon Kim, Minho Shong, Koon Soon Kim, Hyon-Seung Yi
Scientific Reports.2017;[Epub] CrossRef - Growth differentiation factor 15 as a predictor of adverse renal outcomes in patients with immunoglobulin A nephropathy
Ki R. Na, Yoo H. Kim, Hyo K. Chung, Min‐Kyung Yeo, Young R. Ham, Jin Y. Jeong, Koon S. Kim, Kang W. Lee, Dae E. Choi
Internal Medicine Journal.2017; 47(12): 1393. CrossRef - GDF15 contributes to radiation-induced senescence through the ROS-mediated p16 pathway in human endothelial cells
Hyejin Park, Chun-Ho Kim, Jae-Hoon Jeong, Myungjin Park, Kwang Seok Kim
Oncotarget.2016; 7(9): 9634. CrossRef - GDF-15 and Hepcidin Levels in Nonanemic Patients with Impaired Glucose Tolerance
Mehmet Muhittin Yalcin, Alev Eroglu Altinova, Mujde Akturk, Ozlem Gulbahar, Emre Arslan, Damla Ors Sendogan, Ilhan Yetkin, Fusun Balos Toruner
Journal of Diabetes Research.2016; 2016: 1. CrossRef - Cardiac‐Secreted Factors as Peripheral Metabolic Regulators and Potential Disease Biomarkers
Colleen M. Dewey, Kathryn M. Spitler, Jessica M. Ponce, Duane D. Hall, Chad E. Grueter
Journal of the American Heart Association.2016;[Epub] CrossRef - Determinants of growth differentiation factor 15 in patients with stable and acute coronary artery disease. A prospective observational study
Serdar Farhan, Matthias K. Freynhofer, Ivan Brozovic, Veronika Bruno, Birgit Vogel, Ioannis Tentzeris, Sabina Baumgartner-Parzer, Kurt Huber, Alexandra Kautzky-Willer
Cardiovascular Diabetology.2016;[Epub] CrossRef - Effect of Atorvastatin on Growth Differentiation Factor-15 in Patients with Type 2 Diabetes Mellitus and Dyslipidemia
Ji Min Kim, Min Kyung Back, Hyon-Seung Yi, Kyong Hye Joung, Hyun Jin Kim, Bon Jeong Ku
Diabetes & Metabolism Journal.2016; 40(1): 70. CrossRef - Association between Growth Differentiation Factor 15 (GDF15) and Cardiovascular Risk in Patients with Newly Diagnosed Type 2 Diabetes Mellitus
Min Young Shin, Ji Min Kim, Yea Eun Kang, Min Kyeong Kim, Kyong Hye Joung, Ju Hee Lee, Koon Soon Kim, Hyun Jin Kim, Bon Jeong Ku, Minho Shong
Journal of Korean Medical Science.2016; 31(9): 1413. CrossRef - Comparison of Transcriptome Between Type 2 Diabetes Mellitus and Impaired Fasting Glucose
Ying Cui, Wen Chen, Jinfeng Chi, Lei Wang
Medical Science Monitor.2016; 22: 4699. CrossRef - Letter: GDF15 Is a Novel Biomarker for Impaired Fasting Glucose (Diabetes Metab J2014;38:472-9)
Bo Kyung Koo
Diabetes & Metabolism Journal.2015; 39(1): 82. CrossRef - Relationship between hepcidin and GDF15 in anemic patients with type 2 diabetes without overt renal impairment
Jun Hwa Hong, Yeon-Kyung Choi, Byong-Keol Min, Kang Seo Park, Kayeon Seong, In Kyu Lee, Jung Guk Kim
Diabetes Research and Clinical Practice.2015; 109(1): 64. CrossRef - Response: GDF15 Is a Novel Biomarker for Impaired Fasting Glucose (Diabetes Metab J2014;38:472-9)
Jun Hwa Hong, Bon Jeong Ku, Minho Shong
Diabetes & Metabolism Journal.2015; 39(1): 84. CrossRef - Is GDF15 a Novel Biomarker to Predict the Development of Prediabetes or Diabetes?
Kyu Yeon Hur
Diabetes & Metabolism Journal.2014; 38(6): 437. CrossRef
- Effect of a 6-Week Carbohydrate-Reduced High-Protein Diet on Levels of FGF21 and GDF15 in People With Type 2 Diabetes
- Maintenance of Insulin Therapy by Desensitization in Insulin Allergy Patient.
- Jun Hwa Hong, Ji Hye Lee, Jong Ho Shin, Dong Pil Kim, Bong Suk Ko, Byung Joon Kim, Hyun Jin Kim, Kang Seo Park
- Korean Diabetes J. 2008;32(6):529-531. Published online December 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.6.529
- 2,249 View
- 26 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Allergic reaction to human insulin is uncommon. But they can cause mild to severe symptoms such as dyspnea, hypotensive shock, etc. Here we report the case of a patient with type 2 diabetes and insulin allergy successfully managed with desensitization. A 60-year-old man with insulin allergy was transferred. He had poorly controlled type 2 diabetes (fasting blood glucose 230 mg/dL). He developed itching sense and erythema at the injection sites of human insulin in a few minutes. And serum IgE level was elevated to 1618.0 IU/mL. The insulin was changed to other preparations, including short and long-acting insulin analogues, with similar responses. He was commenced on twice a day injection protocol in addition to his oral hypoglycemic agents, and achieved fair control (fasting blood glucose 100 mg/dL) on 24 units of Novomix Flex Pen per day, with little or no skin or systemic reaction. This is the case report of insulin allergy in type 2 diabetes being successfully managed by desensitization.
-
Citations
Citations to this article as recorded by- Allergic reaction to recombinant human insulin
Seong Jin Choi, Min Kwan Kwon, Moon Park, Soo Ya Bae, Hyun Ho Oh, Jong Ho Lee, Ji In Moon, Chan Sun Park, Jong Chul Won, Kyung Soo Ko, Byoung Doo Rhee, Jung Min Kim
Allergy, Asthma & Respiratory Disease.2015; 3(4): 302. CrossRef - Two Cases of Allergy to Insulin in Gestational Diabetes
Gi Jun Kim, Shin Bum Kim, Seong Il Jo, Jin Kyeong Shin, Hee Sun Kwon, Heekyung Jeong, Jang Won Son, Seong Su Lee, Sung Rae Kim, Byung Kee Kim, Soon Jib Yoo
Endocrinology and Metabolism.2015; 30(3): 402. CrossRef - Successful Management of Insulin Allergy and Autoimmune Polyendocrine Syndrome Type 4 with Desensitization Therapy and Glucocorticoid Treatment: A Case Report and Review of the Literature
Joselyn Rojas, Marjorie Villalobos, María Sofía Martínez, Mervin Chávez-Castillo, Wheeler Torres, José Carlos Mejías, Edgar Miquilena, Valmore Bermúdez
Case Reports in Immunology.2014; 2014: 1. CrossRef - Clinical applications of drug desensitization in the Asia-Pacific region
Bernard Yu-Hor Thong
Asia Pacific Allergy.2011; 1(1): 2. CrossRef
- Allergic reaction to recombinant human insulin
- A case of Rhino-Orbital Mucormycosis in Newly Diagnosed type 1 Diabetic patient.
- Jae Min Lee, Kyu Yuop Hwang, Gi Young Choi, Hyo Jung Nam, Dong Hyun Seo, Sun Hyun Park, Jun hwa Hong, Hyun Jin Kim, Kang Seo Park
- Korean Diabetes J. 2005;29(5):495-499. Published online September 1, 2005
- 1,126 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Rhino-orbital mucormycosis was a rare, but mostly fatal fungal infection, usually found in poorly controlled diabetics or other immunocompromised hosts. This fungal infection begins from the nose, and rapidly spreads to the paranasal sinus (PNS), orbits and central nervous system(CNS), and finally extends to the entire organ. Early diagnosis and treatment is the only way to increase the survival rate. Herein Is reported We experienced a case of rhino-orbital mucormycosis, with type 1 diabetes mellitus, which was confirmed by a maxillary sinus biopsy. A 38-year-old male had been frequently treated for tonsillitis, but with no history of diabetes mellitus. He was admitted with mental change, accompanied by a fever, facial tenderness and swelling, with progressive visual acuity loss. During admission, CT and MRI of the in orbital area were performed. A biopsy in of the nasal cavity was also performed, and the mucormycosis was diagnosed through the pathological finding. The patient was treated with intravenous amphotericn B and an endoscopic antrostomy.

 KDA
KDA
 First
First Prev
Prev





